Radiology
- Lobar or segmental density
- Air bronchogram - presence of air bronchogram confirms an alveolar process
- Insignificant loss of lung volume





- A density - representing lung devoid of air
- Loss of lung volume










Chest
-
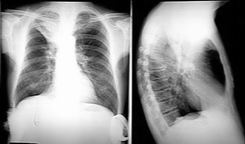
PA
| Who, What, Why? | |
| Prior imaging | oldest & most recent |
| Technical quality | Rotation (spinous processes equidistant from medial end of clavicles)
Inspiration (6 - 7 anterior ribs in MCL) Penetration (spinous processes visible) |
| Lines, tubes | ETT: 5 cm sup to carina [just sup to arch] [has excursion +/- 2 cm] Trachoeostomy tube tip: 1/2 to 2/3 from stoma to carina CVC: SVC (if RA → may arryth or perforatn) S-G: < 2 cm lat to hila NGT: > 10 cm w/n stomach FT: lig of Trietz
Neonate: |
| Abdomen | Diaphragm, pneumoperitoneum, colonic interposition, costophrenic angles, subpulmonic effusion (highest point of hemidiaphragm displaced laterally), tension pneumothorax |
| Thoracic cage | #'s, lesions, notching, pneumothorax |
| Mediatinum | Heart (size, contour), great vessels, airways, esophagus, LN's, AP window, paratracheal stripe, paraspinal lines, ant & post junction lines, azygoesoph recess |
| Lung parenchyma | CPA, apices, volumes, vascular markings, lesions (including behind heart & diaphragm), pneumothorax |
Lateral: diaphragm, CPA, spine sign, hilar LAD, posterior wall of bronchus intermedius, upper lobe bronchi, retrosternal space


-
Opacity
Etiologies: Blood, pus, fluid, cells, protein
Common findings in ICU: edema, atelectasis, effusion, cardiomegaly, life supports
Cardiogenic pulmonary edema progession:
® vascular redistribution
® interstitial pulmonary edema (perihilar haze, peribronch cuffing, Kerley A & B lines)
® alveolar pulmonary edema
® pleural effusion
| Air-space disease | Fluffy margins
Acinar shadows (7 mm) Air bronchograms Silhouette sign Homogeneous (when acinar consolidation confluent) Non-segmental distribution (d.t. intersegmental channels) |
| Interstitial disease | Ground-glass (granular)
Reticular (fine, medium, coarse; Kerley A, B, C lines; acute: hazy, not distorted; chronic: sharp, distorted) Nodular Reticulonodular Honeycomb (5 - 10 mm) |
| Atelectasis | Volume loss, no air bronchograms if resorption atelectasis
Resorption (e.g. d.t. mucus plug) Relaxation (passive) Adhesive (e.g. d.t. abnl surfactant) Cicatrization (d.t. pulmonary fibrosis) |
| Benign Nodule | Size: <2 cm
Margins: well-defined, smooth Calcification: laminated, multiple punctate, or popcorn Fat indicates hamartoma Growth: none over 2 yrs Age: below 40 y/o |
Pleural Effusion
Can see 25 mL on lat decub
Can see 300 mL on PA
Mediastinal Masses
| Anterior | Thyroid
Thymoma Teratoma Terrible lymphoma |
| Middle | Lymphadenopathy
Esophageal mass Hernia, Hematoma Aneurym Bronchogenic cyst Inflammation (sacoidosis, T.B., histoplasmosis, coccidioidomycosis) Tumor |
| Posterior | Aneurysm
Neurogenic tumor Spine mass |
Aortic Disruption
left Bronchus depressed
left pleural Effusion
widened Mediastinum
apical Cap
Aortic knob indistinct
Trachea deviated to right
Asbestos-related pleural disease: pleural plaques, diffuse pleural thickening, pleural calcification, benign effusion
Pleural calcification without h/o surgery, TB, empyema, hemothorax, etc. is pathognomonic of asbestos exposure.
Asbestosis is asbestos-related interstitial pulmonary fibrosis
 
|  
|

| 
|
Etiology
Post-obstructive Atelectasis
Etiology
Pneumothorax
Lung Mass
Pleural effusion
Cavity
Congested lungs
In CHF, there is progression from
Chest wall lesion
Solitary pulmonary nodule
Lymphadenopathy
Diffuse lung disease
Diffuse interstitial pattern
Common etiology
Diffuse alveolar pattern
Chronic:
Mediastinal mass
Common Mediastinal masses in the anterior mediastinum
Mediastinal Lymphadenopathy
Etiology
Lesions of apices of Lungs
Multiple diffuse nodules
Granulomatous diseases:
Miliary TB
Multiple mass lesions
Bronchial:
Lung abscess
Common segments where aspiration lung abscess occurs:
Etiology for Lung abscess:
Diffuse alveolar infiltrates
Soft fluffy lesions
Bullous Emphysema
Etiology
Loculated Empyema
Inlet to outlet sign:
Inlet to outlet shadow





























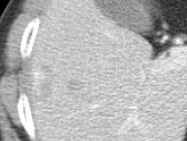
Consolidation
Opacification
Lobar/Segmental distribution
Air bronchogram
No significant loss of lung volume
Streptococcus
Legionella
Mycoplasma
Opacity (airless lung)
Signs of loss of lung volume:
Mediastinal shift
Elevated diaphragm
Movement of fissures
Shift of hilum
Change of proportion of lungs
Smaller hemithorax
Compensatory hyperinflation
Cancer
Foreign body
Benign tumor
Granuloma
Dark field with no vascular markings in the pleural space
Visible collapsed lung
Larger hemithorax
Etiology
All Lung Diseases
Trauma
Procedures
Barotrauma (Ventilator)
Bullous lesions
Marfan syndrome
Ehler Danlos syndrome
Catamenial Pneumothorax
Homogenous liquid density
Density >5 cm diameter (less than 5 cm is called pulmonary nodule)
Sharp margins
No respect for segments or fissures
Etiology
Lung cancer
Granulomatous infections (TB, Histo,Blastomycosis)
Wegners Granuloma
Rheumatoid lung
Metastasis
Loss of costophrenic angle
Loss of diaphragmatic shadow
Homogenous opacification
Shift of mediastinum to opposite side
Ellis line
Etiology (common diseases)
Congestive heart failure
Cancer
Tuberculosis
Empyema
Hemothorax
Etiology
Lung cancer: Squamous cell cancer Lung (Thick wall, Irregular lumen, Stalactites and Stalagmites)
Metastasis
Wegners Granuloma
Rheumatoid lung
Cystic fibrosis
Granulomatous infections TB, Histo
Lung abscess
Necrotizing Pneumonia
Coccidiomycosis
Fungous ball (Mobile ball inside a cavity)
Vascular congestion (recognized as prominent pulmonary veins)
cephalisation.
Next, interstitial edema and increased lymph flow manifests itself as Kerley lines.
Next, basal congestion with smaller lungs due to increased elastic recoil. Congested, boggy Liver also pushes the diaphragm up.
Lastly, full-blown pulmonary edema: acute diffuse alveolar pattern
Peripheral density
Sharp inner margin
Indistinct outer margin
"Cat under the rug" appearance with shallow concave edges.
Etiology
Expanding rib lesions
Fracture with hematoma
Callus
Metastasis
Plasmacytoma
Parietal pleural masses (mesothelioma)
Neurofibroma
Plumbage
Liquid density
Distinct margin
Between 2-5 cm diameter
Oval or round
no other lesions
Etiology
Cancer
Benign tumor
Granulomas
Rare but characteristic conditions:
AVM
Rheumatoid nodule
Round atelectasis
Hydatid cyst
Polycyclic margin
Clear space between heart and the nodal density with hilar nodes
Extrapleural sign with mediastinal nodes
Widening of mediastinum
Etiology
Cancer Lung
Lymphoma
Granulomatous diseases
TB
Sarcoidosis
Histoplasmosis
Silicosis
categorized into
Alveolar
Interstitial
Vascular
Most of the time, mixed and difficult to categorize into one pattern.
Lines (Kerley lines)
Nodules
Honeycombing
Granulomatous disease
Miliary TB
Sarcoidosis
Silicosis
Lymphangitic spread
Idiopathic fibrosis
Drug induced fibrosis
Butterfly or medullary distribution
Lobar or segmental densities
Soft fluffy coalescing densities
Air bronchogram
Alveologram
Common causes
Acute:
Water
Blood
Inflammatory exudate
Alveolar proteinosis
Alveolar form of Lymphoma
Alveolar form of Sarcoidosis
Alveolar form of TB
Fungal infections
Mineral oil aspiration
Desquamative interstitial pneumonia
Homogeneous liquid density
Distinct margin
Mediastinal because has Extrapleural sign (peripheral, absence of one of the margins both in PA and lateral view)
Location is suggested by x-rays to be anterior mediastinum
Thymoma
Teratoma
Thyroid
Testicular metastasis
Terrible lymphoma
Widening of Mediastinum
Polycyclic margin indicating that they are multiple nodes
Widening of Carina with subcarinal nodes
Lymphoma
Cancer Lung
Granulomatous diseases
Castleman's disease
Common diseases:
Tuberculosis
Pancoast tumor
Components of Pancoast tumor
Apical shadow
Destruction of posterior 1st and second rib
Horner's syndrome
Brachial plexus involvement
In the CXR you cannot recognize Horner's and brachial plexus involvement (sometimes shoulder sags on that side).
You should always take a very close look at ribs for destruction. If it is present most likely it is cancer.
Sarcoidosis
Histoplasmosis
Silicosis
Eosinophilic granuloma
Metastasis from Thyroid
Alveolar cell carcinoma
Whenever you see multiple mass lesions considerations are either the disease process is at the end of vessel or bronchus, as both of them branch and reach lung tissue.
Vascular:
Tumor emboli/Metastasis
Septic emboli
Vasculitis/Wegners granuloma
Aspiration
Tumor emboli are in the interstitum and there is no inflammation, hence the margins of the mass lesions are sharp.
Any time you see a fluid level in a cavity, the most likely diagnosis is Lung abscess. I am not even going to give you other uncommon causes.
Axillary subbasement of anterior and posterior RUL segments
Superior segment of RLL
Superior segment of LLL
These three segments will account for 85-90% of all aspirated lung abscesses. This is determined by patients position at the time of aspiration. Gravity determines which segment the aspirate will end up in.
Endobronchial lesion
Deglutition problem
Esophageal disease
Coalescing lesions
Air bronchogram
Butterfly/Medullary distribution
Cortical distribution
Alveologram
Segmental/Lobar density
Etiolgy of Chronic alveolar infiltrates.
Alveolar proteinosis
Alveolar form of Sarcoidosis
Alveolar form of TB
Alveolar form of Lymphoma
Psudolymphoma
Alveolar cell carcinoma
Mineral oil aspiration
Alveolar pattern of metastases
Look for avascular regions, hyperlucent areas.
Lines that do not correspond to known fissures could be walls of blebs.
Bullae become evident when there is Pneumothorax, look carefully along the pleural surface of atelectatic lung.
In routine Emphysema
Bullous emphysema (No airway obstruction)
Homogenous density
Often mistaken for consolidation or Pleural effusion
Criteria for lobar consolidation or Pleural effusion not met
Lines not corresponding to fissures
Lateral view most helpful
Structures traversing from inlet to outlet of Thorax
Aorta on left
Esophagus on right
Widening of mediastinum
Inhomogeneity of cardiac density
Etiolgy
Dissecting Aneurysm of Aorta (The wavy margins is suggestive of dissection of Aorta)
Right sided Aortic arch
Achalasia of Esophagus
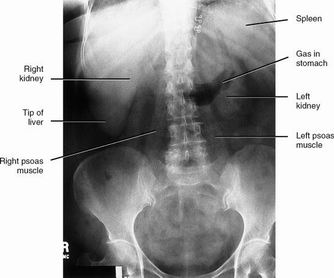
Abdominal
| Prior imaging | oldest & most recent |
| Lines, tubes | E.g. NGT, Dubhoff feeding tube |
| Stones | Nephrolithiasis, cholelithiasis |
| Bones | Ilioishial line, iliopectineal line, arcuate lines, Shenton's arc, coxa vara or valgus, protrusio acetabuli, anterior & posterior rim lines, femoral head, bone texture, joints |
| Mass | |
| Gas | Obstruction, ileus |

| 
|
|
|

| 
|

|  
|
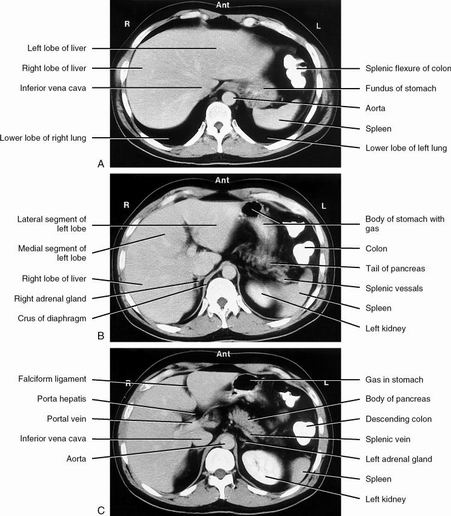
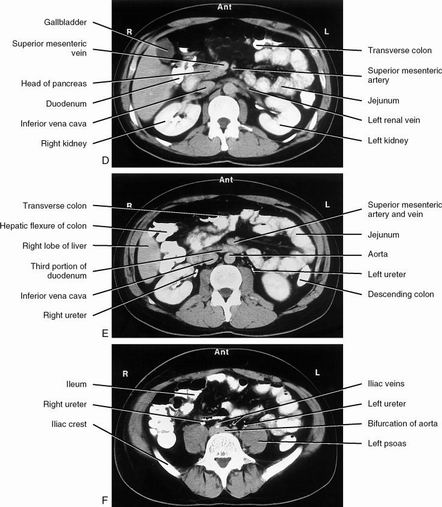
| Arterial phase & portal venous phase | |
 
|  
|

| |

| 
|
Musculoskeletal
-
Stability = Propensity to further displacement
Fractures
| Prior imaging | oldest & most recent |
| Location | E.g. proximal, middle, distal third |
| Type | E.g. transverse, oblique, spiral, comminuted, green stick, torus, stress, insufficiency |
| Joint involvement | |
| Displacement | E.g. 50% posterior |
| Angulation | E.g. vertex medial |
| Rotation | |
| Over-riding / distraction | |
| Effusions | |
| Soft tissue swelling | |
| Hardware | Correct positioning, lucencies, osteomyelitis, #'s
E.g. intramedullary rod, dynamic hip screw, spinal fusion plate & screws, k-wires, cortical screws, cancellous screws,cerclage wire, tension band wire, external fixator Orthopedic hardware |
Tooth Numbering System

C-Spine
| Prior imaging | oldest & most recent |
| Bodies | Height, trabeculations |
| Disks | Height, |
| Odontoid | #'s, dens-anterior arch distance (adults: < 3 mm; peds: < 5 mm) |
| Lines | Anterior spinal line, posterior spinal line, spinolaminar line, clivus base line |
| Lordosis | |
| Soft tissue swelling | Retropharyngeal, retroesophageal |
Degenerative Disease of Spine
| Degenerative disk disease (DDD) | ↓ disk space osteophytes borders of adjac vert bodies may vacuum phen |
| DISH | flowing ossifn >= 4 contig verts no facet or SIJ ankylosis rel minimal DDD |
| Spondylosis deformans | ant & lat osteophytes rel preserved disk spaces |
| Facet DJD | osseous facet overgrowth ↓ jt space sclerosis |
Facet DJD + DDD may → degen spondylolisthesis
Scheuermann's disease
- Categorized as an "osteochondrosis"
Possibly a growth disorder of vertebral bodies (poorly understood)
Typically 13-17 y/o with back pain
Lower thoracic spine involved most frequently
- Radiographs:
Multiple Schmorl's nodes
Disk space narrowing
Endplate irregularities
Anterior wedging
Changes seen in >3 vertebral bodies (with > 5 degrees anterior wedging in each)
Kyphosis usually > 35 degrees


Shoulder
| A-C joint | 3 - 8 mm |
| Coracoid - clavicular distance | 10 - 13 mm |
| Glenoid - humeral distance | ?8 mm |
Acetabulum
Ileopectineal Iileopubic) line
Ileoischial line
Tear drop
Posterior rim
Superior rim
Anterior rim
Ankle Fracture
Medial malleolus
Lateral malleolus
Posterior malleolus
Base of 5th metatarsal
Dome of talus
Lateral talar process
Anterior calcaneal process
Lateral calcaneal process
Proximal fibula
Soft tissue swelling
Arthritides
| Osteoarthritis
"Wear & tear exceeds repair." | Subchondral sclerosis
Osteophytes Asymmetric joint space narrowing Pseudocysts |
| Rheumatoid arthritis | Erosions
Symmetric joint space narrowing Soft tissue swelling Osteopenia (periarticular) |
| Charcot joint | Joint destruction
Heterotopic bone formation Subluxations |
Bone Tumors
Margins
| I - Geographic | A - well-defined & sclerotic B - well-defined & not sclerotic C - ill-defined | usually benign usually benign not ... |
| II - Moth-eaten | ||
| III - Permeated | ||
Periosteal Reaction
Aggressive: sunburst, hair-on-end, Codman triangles, laminated
Osteomyelitis
Plain films (require 10-14 days to develop):
-
STS
Periosteal reaction
Lytic changes (Require 2-6 weeks and reflect 50-70% bone density loss. Antibiotic use may arrest bone mineral loss.)
-
Can diagnose osteomyelitis within 3 days of symptom onset. 95% sensitive and specific.
False positives: healing fractures, prostheses, neuropathic osteoarthropathy.
In this instance, Indium-labeled WBC images are superimposed on the bone scan.
Spine




| |

| 
|

| 
|

| 
|

| 
|

| 
|

| |

| 
|

| 
|

| 
|
|  |

| 
|

| |